This blog post is part of our Policy Pulse series, which spotlights crucial policy issues in independent and community-based primary care, along with potential solutions from Aledade’s Policy team.
Aledade recognizes investment in primary care to be at the core of our work and a critical component to ensuring long-term sustainability of independent and community-based primary care. Unfortunately, across the country, there is an underinvestment in primary care.
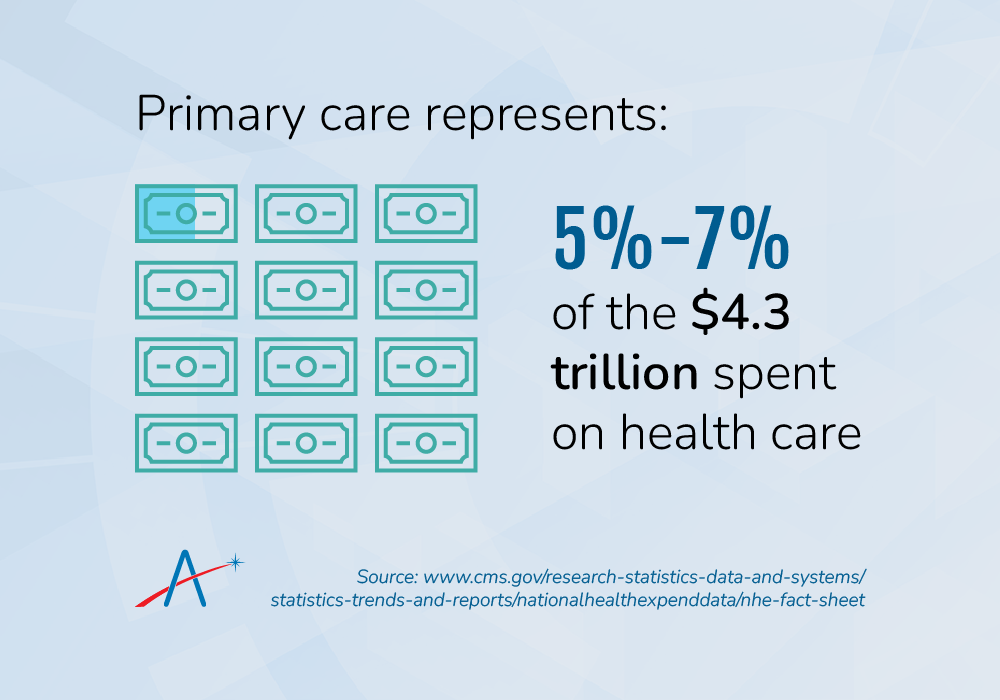
Across states, primary care spending makes up only about 5%-7% of total health care expenditures in the United States. This is about half of the average spending on primary care among OECD countries. In order to reduce health care costs and improve outcomes, we need to increase our investment in primary care and establish minimum primary care spending targets for payers.
State minimum primary care spend legislation can be a meaningful tool to reorient the focus of our health care system toward primary care. By establishing clear definitions and targets for primary care spending as a proportion of a health plan’s health care expenditures, minimum primary care legislation provides regulators with tools to increase transparency and accountability for primary care spending.
Creating a system for measuring and reporting primary care spending enables health plans to better understand their own spending patterns and identify areas where they can improve efficiency and reduce costs. Strong comparative data can help foster competition between plans, driving primary care spending.
Key tasks in establishing a minimum primary care spend framework:
- Defining primary care: The first challenge policymakers and advocates face in establishing minimum requirements for primary care spending is defining primary care. Definitions of what services count as primary care can vary state-to-state, which can complicate comparisons across states. Establishing standard definitions and tracking a range of spending can help mitigate complications and more accurately assess the levels of primary care spending in a state.
- Addressing increased spending or reallocation of spending: Increased primary care spending comes with its own short-term economic and political realities. Increasing primary care spending may mean an increase in overall spending or a reallocation of resources from different sources (e.g., specialties within hospital systems), which can create some tension. Data shows that in the long term, robust primary care can help reduce costs and free up resources for additional investments to strengthen the health care system and further innovations in care delivery.
- Minimizing administrative burdens for primary care practices: In drawing up minimum primary care legislation, policymakers should take into consideration administrative burdens for small practices and community-based clinics and as well as the ongoing pattern of practice consolidation. Minimum primary care spend laws should be crafted in such a way that ensures data requirements from payers and other entities on primary care spending does not create cumbersome data collection and reporting requirements for these practices.
- Creating authority and clarity for enforcement: Establishing authority and clarity is critical for effective minimum primary care spend legislation. Some states have only set voluntary goals and/or are measuring spending with no penalties or enforcement actions. In other cases, enforcement actions are unclear. Further, in many cases self-funded/non-fully insured plans are exempt from state enforcement for primary care spending targets under the Employee Retirement Income Security Act (ERISA). This means that state regulators may only have authority to enforce spending targets for a fraction of plans in the state. States could explore potential ERISA “end around” solutions, such as requiring payers to put funds into a pool and then distributing that pool to primary care providers.
So far, a number of states have made efforts to set targets for minimum primary care spending. State-based payment reform collaboratives have proliferated as a way to study and provide recommendations on primary care spending to state policymakers and allow for collaboration between primary care providers, health plans and other stakeholder groups.
Aledade supports efforts to establish state minimums for primary care spending and believes that input from primary care clinicians is critical to ensuring this legislation is rooted in patient outcomes and bolsters the sustainability of independent practices and community-based clinics.
Minimum primary care spend should also be part of a broader effort to develop payment models that incentivize primary care, as well as encourage clinicians to move into value-based care and accountable care models to improve patient outcomes and reduce costs.
Resources:
- Blog: Investing in Primary Care Is Critical to Improving the Health of Communities
- Policy Brief: What is Minimum Primary Care Spend?
- Infographic: 2021 PCP MSSP Savings and Quality Results
- Article: Primary Care in High-Income Countries: How the United States Compares
- Article: Primary Care Visits Increase Utilization of Evidence-Based Preventative Health Measures
- Report: Investing in Primary Care: Lessons from State-Based Efforts



