Independent Physicians Thriving in Transition to Value

The comment period for Medicare’s proposed rule on the Quality Payment Program closed last night, so as usual we’ll take this opportunity to share our full comments on the proposed updates to how Medicare shapes the path to a value-based future.
August 21, 2017
Seema Verma, Administrator
Centers for Medicare & Medicaid Services
7500 Security Blvd
Baltimore, MD 21244
Re: CMS-5522-P: Medicare Program, CY 2018 Updates to the Quality Payment Program
Dear Administrator Verma:
Aledade partners with 205 primary care physician practices, FQHCs and RHCs in value-based health care. Organized into 16 accountable care organizations across 15 states, these primary care physicians are accountable for more than 190,000 Medicare beneficiaries. More than half of our primary care providers are in practices with fewer than 10 clinicians. We are committed to outcome based approaches to determine the value of health care. We are committed to using technology, data, practice transformation expertise and most importantly the relationship between a person and their primary care physician to improve the value of health care.
Creating a path for independent practices to thrive in the transition to value-driven health care
- Whole hearted endorsement of the inclusion of “the preservation of independent practices as a guiding principle for the Quality Payment Program (QPP)”
- Virtual groups provide a needed step on the path to transition to value-driven health care by allowing independent practices to come together for QPP even if they are not ready to take on the total cost of care
- Virtual groups are part of the path to value-driven health care that must be carefully crafted to be attractive to independent physicians
- The low volume threshold proposal leaves too much of the Medicare spend and therefore too many Medicare beneficiaries out of the program. We recommend that no more than 10 percent of the Medicare Part B spend should ever be excluded from QPP.
Measuring QPP performance and reducing administrative burden
- We recommend that the cost category for total cost of care be included for 2018.
- We recommend that the AAPM bonus move forward a year with bonuses earned in 2018 paid in early 2019 or even in 2018 itself
- We recommend that CMS value simplicity and minimizing administrative burden above other characteristics of the all-payer determination for APMs
Below is a full explanation of those positions. Thank you for your consideration as we move together through this exciting time in health care. Please feel free to contact Travis Broome ([email protected]) if you or your staff have questions or would like to explore these positions further.
Sincerely,
/s/
Farzad Mostashari, MD
CEO and Co-Founder, Aledade, Inc
Independent Physicians Thriving in Transition to Value
Principle of Independent Practice
It would be difficult to overstate the importance of CMS’s inclusion of the preservation of independent practices as a principle of the QPP. Independent physician practices have proven to be the most successful in accountable care[1] and key to maintaining competitive health care markets.[2] The same characteristics that make the independent physician practices successful also make this principle particularly challenging for CMS to deliver on. Physicians must feel the change in their practice. There is no board room in small practices where a government affairs team will explain slight tweaks in policy that increase revenue by a half a percentage point. The preservation of independent practice in QPP will be felt by CMS’s continuous effort to reduce the administrative burden of participation in QPP through technology, policy and measure design and a continuous effort to link performance with incentives as tightly as possible.
Virtual Groups
We support CMS’s proposal for virtual groups. CMS specifically asked for comment on several additional requirements for virtual groups. We do not believe that at the onset it is advisable to set additional standards on virtual groups. We recommend the following principles to guide CMS’s finalization of the virtual groups.
- Voluntary election by physicians to be in a virtual group prior to the start of the performance year
- Agree to work together to improve their performance in QPP
- Must agree to be scored on quality
- Can elect to be scored on
- Clinical Practice Improvement Activities
- Advancing Care Information
- Resource Use
- Can utilize any reporting method including Group Practice Reporting Option (GPRO)
- Identify to CMS the officer responsible for the virtual group’s reporting
- The virtual group is responsible for ensuring group reporting (i.e. CMS should not be responsible for aggregating the data across practices except in the area of resource use and other claims based measures)
CMS has proposed that all virtual groups would be scored on all categories as a group. We believe that this could be a limiting approach. For example, it would dissuade any virtual group from admitting members who do have 2014 Certified EHR Technology due to the effects on the advancing care information score.
Finally, we recommend that CMS allow third-party entities to organize and report for QPP on behalf of smaller practices. The practices making up the virtual group should not be required to manage this process internally.
Successful Transition to Value Based Care
We continue to work together with CMS to define a path that both transitions to value based health care and preserves independence.
It is helpful to remember what the path looked like just 5 years ago:
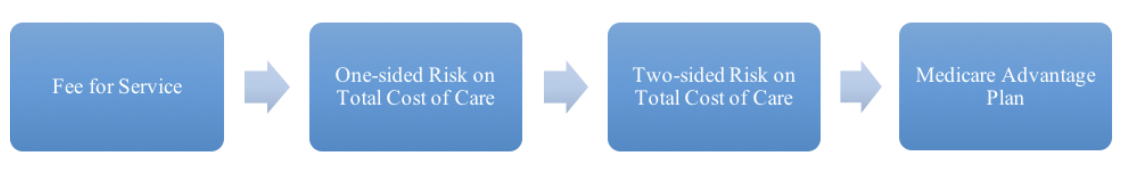
These are all huge leaps. First, physicians must take responsibility for total cost of care in a way they never had before. Second, they must take on a level of risk that could ruin an independent practice. Third, they must develop health insurance operations. The size of those leaps simply prevents many physicians from taking the next step.
Today, with the proposal in this rule for virtual groups the path looks more achievable:
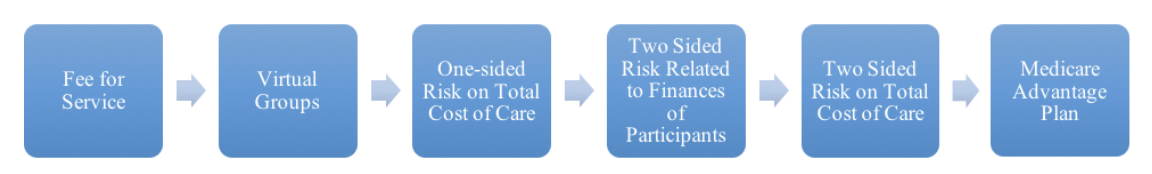
With this proposed rule CMS has smoothed out the move from FFS to total cost of care. In prior regulations, CMS made incremental progress on the move from one-sided risk to two-sided risk. While not specifically for this regulation, we recommend a path to CMS that bases risk on the financial wherewithal of the participants in the total cost of care model and lets physicians move to Medicare Advantage to assume full risk without the burden of claims processing and network development. Our recommendations for the former can be found in the blog for the American Journal of Managed Care[3] and for the latter in the blog for Health Affairs[4].
Our recommended path is:

We believe this path is ideal for encouraging independent practices to continue to make the transition to value based care where they have proven they can succeed at all levels in various pockets of the county. We know they can succeed not just here and there, but in nearly every health care market in the country.
Low Volume Threshold
CMS has proposed to raise the low-volume threshold to exclude individual MIPS-eligible clinicians or groups who bill less than $90,000 Part B billing OR provide care for less than 200 Part B enrolled beneficiaries. We do not support raising the low-volume threshold, and recommend maintaining the current policy of excluding clinicians or groups who bill less than $30,000 to Part B or care for less than 100 Part B enrolled beneficiaries.
In the transition year final rule, CMS estimated that about 32.5 percent of providers would be exempt from MIPS because they do not meet the low-volume threshold, but the number of providers actually exempted for 2017 was higher than anticipated. The increased low-volume threshold creates an arbitrary cut-off for performance in the MIPS program without first assessing the impact of the current low-volume threshold on Part B providers. CMS should continue to transition a greater percentage of total Medicare spend away from fee-for-service to payment arrangements that account for quality, cost, and patient outcomes, rather than further reducing the number of providers eligible to participate.
Further, the modified threshold would mean that some clinicians who were eligible to participate in 2017 will be excluded from MIPS in 2018. We recommend that CMS extend the option for clinicians to voluntary participate in MIPS reporting in 2018 for a performance score and performance-based payment adjustment. Clinicians who made investments and preparations to participate in MIPS during the transition year should not lose out on the opportunity to earn a positive payment adjustment in 2018.
QPP Measurement AAPM Determination
Resource Use Category
Aledade supports a transition to value-based payments that hold providers accountable for patient experience, quality of care, and total cost. By statute, in the QPP’s third performance year, the cost performance category must be weighted at 30 percent and the MIPS performance benchmark must be set at either the mean or the median score of all MIPS participants. Introducing cost performance into the MIPS score should be done incrementally, rather than creating a steep cliff from 0 percent weight in PY2 to 30 percent in PY3. Therefore, Aledade does not support reweighting the cost performance category to 0 percent of the final score, and recommends this category be weighted to at least 10 percent of the final score.
Measuring cost is an integral part of measuring value because clinicians play an important role in managing care so as to avoid unnecessary services. We appreciate the ongoing CMS efforts to better align the episode cost measures across programs and to better attribute beneficiaries to specialists for purposes of QPP. However, the lack of finality in these efforts should not slow the inclusion of total cost of care in QPP for 2018.
Aligning the AAPM 5 Percent Incentive with Action
Currently, a physician chooses to join an AAPM in the summer of 2017 (CMS’s 2018 deadline for the Medicare Shared Savings Program was July 31st), they participate during 2018, they receive their performance in the AAPM in August of 2019 and then they receive their lump sum bonus for participation in the AAPM in May of 2020. Almost three years have passed between a physician’s decision to join an AAPM and the reward for that decision.
When we talk to physicians about AAPM participation they naturally assume that since the 5 percent is contingent only on participation that they will receive the bonus in not May of 2020, but May of 2018 or even sooner. More than one physician has naturally assumed that the bonus would come January 1, 2018. Every minute explaining why this isn’t the case is a minute spent decreasing the likelihood of AAPM participation, the very thing Congress funded the 5 percent bonus to incentivize. While we understand that not all AAPM models require full year participation and therefore within-year bonuses may not be possible, CMS should explore every proxy to bring action and incentive as close together as possible. At a minimum, CMS should use the same year for the QP determination period and the claims period to pay out the bonus the year following participation. So in 2018 participation in AAPM would pay the 5 percent bonus in May 2019 based on the 2018 claims instead of May 2020 based on 2019 claims. To have the bonus for mere participation come seven months after the savings for actual performance in the AAPM strikes physicians as so backwards that it calls into question the credibility of the AAPM itself and negates the positive effects of the 5 percent bonus.
All-Payer AAPM Determinations
As members of the Healthcare Transformation Taskforce (www.hcttf.org), we worked closely with other health care providers, health plans, patient groups and health care payers to make recommendations on this area and we would refer you to those comments for the details.
In our comment letter, we want to emphasize the importance the health care providers place on the simplicity of this process. We do not desire to impose a high administrative burden on either health plans or on CMS in order to make the all-payer AAPM determinations. In this case, we would recommend that CMS value simplicity over every other characteristic of this program.
[1] https://www.nejm.org/doi/full/10.1056/NEJMsa1600142#t=article
[2] https://www.brookings.edu/research/making-health-care-markets-work-competition-policy-for-health-care/
[3] https://www.ajmc.com/contributor/travis-broome/2016/03/changing-stop-loss-formula-can-drive-interest-in-risk-based-models
[4] https://healthaffairs.org/blog/2017/07/06/spurring-provider-entry-into-medicare-advantage/



