Due to the COVID-19 pandemic, since March 2020, all states have provided continuous Medicaid enrollment in exchange for enhanced federal funding. At the end of last year, Congress delinked this provision from the Public Health Emergency, ending continuous enrollment on March 31, 2023. This means as many as 14 million Medicaid beneficiaries could lose coverage – and access to care – in the coming days and months.
While states are on different timelines, they must begin redetermining eligibility for the Medicaid population within 12 months of April 1, 2023, and complete all renewal determinations within 14 months. This is a confusing and scary time for Medicaid beneficiaries who risk losing coverage or are unsure of their status.
“Any patient losing coverage often backslides in treatment, whether it be for diabetes, depression, someone in the middle of a course of treatment for cancer, or any chronic illness,” said Shawn Purifoy, MD, Aledade’s Senior Medical Director and owner of Malvern Family Medical Clinic in Arkansas.
To assist patients, practices and ACOs through this transition, Aledade is taking a three-pronged approach:
- Aledade Staff Education: The Medicaid Strategy team has developed state-specific educational materials and training with Aledade staff who work directly with member practices to ensure they understand how their states are handling redeterminations and the potential impact to patients (i.e., decreased coverage, effects on population health)
- Practice Support: In the coming weeks, practices will experience patients showing up to appointments to find they no longer have coverage. Aledade is educating ACO mem
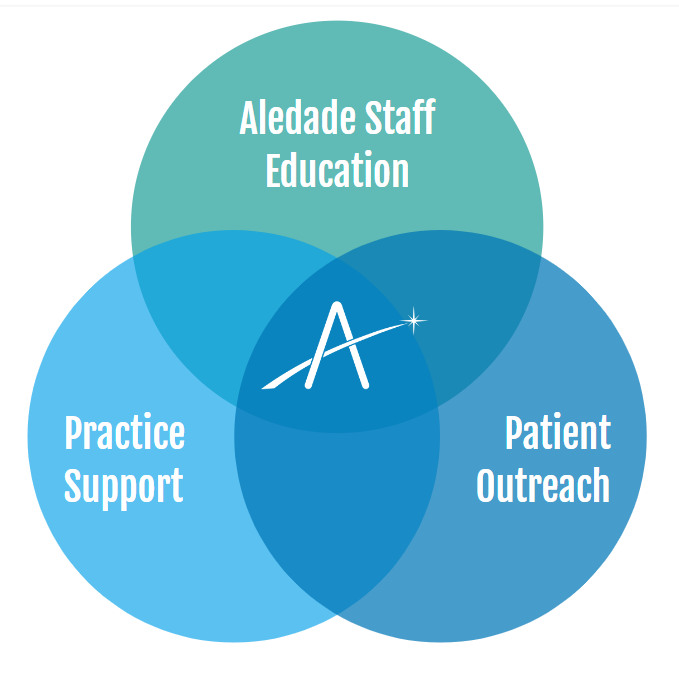 ber organizations about their state’s unique redetermination timeline and process, so practice staff can be an informed resource for patients. The Policy Team also sends regular updates and is available to member practices for direct questions and support.
ber organizations about their state’s unique redetermination timeline and process, so practice staff can be an informed resource for patients. The Policy Team also sends regular updates and is available to member practices for direct questions and support. - Patient Outreach: Medicaid beneficiaries are at risk of losing coverage because they are no longer eligible or for procedural reasons, such as not taking steps to renew their coverage. These individuals will be uninsured, which means there will be more patients putting off care and later going to the emergency department. Aledade is conducting a patient outreach campaign through text and potentially direct mail to reach these patients directly and help them reapply for Medicaid if they are eligible or seek coverage elsewhere.
Aledade’s tailored approach to patient outreach
Aledade’s Medicaid Network Performance and Aledade Care Solutions’ Patient Engagement teams have spent months working with state Medicaid agencies and health plan partners to identify patients who will be affected, and tailor outreach with messaging that aligns with the different states’ campaigns and timelines. The first set of text messages went out in April and will be followed by a second wave in May.
“Our communication strategy prioritizes individuals who are most at risk for losing coverage, because the data shows they have aged out, moved, or had another reason they would be ineligible,” said Chelsea Graves, Aledade’s Director of Medicaid Network. ”We are proactively reaching those individuals to help them make a plan to secure coverage elsewhere. Our state and health plan partners have been instrumental in helping us get the right data and make sure our timing and messaging was consistent with what the state was doing.”
Medicaid “churn:” an ongoing barrier policymakers must address
Even prior to the pandemic, Medicaid churn – or beneficiaries temporarily losing Medicaid coverage because of administrative barriers – has been a major challenge that leads to disruptions in care, worse health outcomes and inefficient, rising health care costs. Research shows that 11.2% of full-benefit children and 12.1% of adults lost coverage in 2019 just to gain it back in 2019.
The paperwork and administrative burdens go beyond bureaucratic disruptions – they endanger people’s health. The Department of Health and Human Services report shows that it is even worse for people with both Medicare and Medicaid: 29% of these dual eligibles transition lose coverage and regain it in a given year. Losing coverage is usually temporary and based on administrative issues (such as complex renewal processes or slight fluctuations in income for a short time).
“At Aledade, we are focused on supporting strong relationships between patients and their primary care team. When patients are confused about coverage or are losing coverage, it puts that relationship – and the patient’s health – at risk,” said Casey Korba, Aledade’s Director of Policy.
This transition in and out of Medicaid makes it much more difficult for primary care practices participating in value-based care models and ACOs to take advantage of the infrastructure and tools they have in place to coordinate care, build trust with patients and outreach to patients who are in care transitions.
For example, research shows when patients are coming out of an inpatient facility such as the hospital, rehabilitation facility or skilled nursing facility, it is critical that the primary care team follow up within a few days so that they manage medicine reconciliation, review discharge information, coordinate follow-up testing or treatment, and educate the patient and family. Patients who do not receive transitional care management service are more likely to be readmitted to the hospital.
“At Aledade, we are focused on supporting strong relationships between patients and their primary care team. When patients are confused about coverage or are losing coverage, it puts that relationship – and the patient’s health – at risk.” – Casey Korba, Director of Policy
The Medicaid and CHIP Payment and Access Commission (MACPAC) has proposed policy changes that would allow states to implement 12-month continuous Medicaid eligibility for the dually eligible population without obtaining a waiver. This would promote continuity of care by having an annual renewal process for dually eligible beneficiaries. Future enrollment strategies should aim for streamlined processes that use available beneficiary data and require less interaction with the Medicaid agency.
Aledade will work with practices, health plans and states to close the gaps today and advocate for policy solutions to close the gaps permanently.
Maintaining and nurturing a strong patient-clinician relationship is critical to primary care. Accountable care models are based on the concept that clinicians accept accountability for managing the full continuum of care for their patients. After the Medicaid redetermination process has concluded in the coming months, providing solutions to patients who risk transitioning out of Medicaid will continue to be top of mind for Aledade and our member practices. We will work with states and health plans partners to support patients.
“No one is closer to the patient than the primary care practices. We are focused on equipping our practices with the data and resources they need to be able to proactively address coverage issues with patients on Medicaid as they come in for care,” Graves said.



