By Rebecca Cooper, Senior Policy Analyst
On October 7, Aledade’s North Carolina Policy Committee hosted a discussion among leaders from the private and public sectors on the importance of supporting independent and community-based primary care practitioners, with a focus on value-based care.
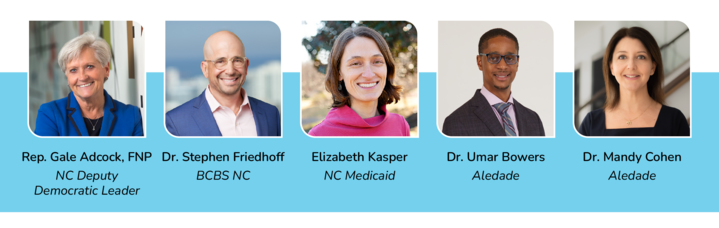
Dr. Mandy Cohen, Aledade’s Executive Vice President and CEO of Aledade Care Solutions, facilitated the first session, a panel discussion, focused on legislative priorities as well as how health plans can work with clinicians to advance value-based care. The panel featured Representative Gale Adcock, FNP, North Carolina’s House Deputy Democratic Leader in District 41, and Dr. Stephen Friedhoff, VP of Health Care Services for BlueCross BlueShield North Carolina. Dr. Umar Bowers, an independent primary care physician and Aledade Medical Director who serves on the Quality Management Committee for one of North Carolina’s Prepaid Health Plans, engaged in dialogue with Elizabeth Kasper, Special Policy Advisor for Alternative Payment Models at North Carolina Medicaid.
How do we support independent NC practitioners who want to provide patient-centered, coordinated primary care?
Independent primary care and community-based practitioners are at the heart of the health care experience and Aledade’s work. North Carolina’s independent primary care practices are at risk from massive health care consolidation, proven to drive up health care costs without improving quality.
In North Carolina, we have 211 enrolled practices, over 2,000 clinicians, and nearly 400,000 attributed patients, and have reduced patients’ health care costs by an average of over $600 per MSSP member. This adds up to big savings for our practices. Since 2019, Aledade ACO members in North Carolina have generated over $80 million in savings in their commercial plans and nearly $76 million for Medicare through their Medicare Shared Savings Program and Medicare Advantage contracts.
Dr. Friedhoff at BCBS NC cited these same facts, saying that value-based care is key to strengthening primary care. He went on to note not only the value in saving the system money, but, equally important, the value and humanity we bring to patients and practices. In the panel, speakers focused on strategies to strengthen value-based care, including through advancing telehealth learnings from the pandemic and reducing administrative burden for clinicians.
Telehealth: real care delivered virtually
When thinking about access to services and different modalities for delivering care, Dr. Friedhoff noted that BCBS NC has covered telehealth services for over 20 years. The organization expanded telehealth codes during the pandemic, and saw a 75-fold increase in telehealth visits. Moving forward, he said that BCBS NC is looking to expand coverage – up to 97% of services, including primary care, behavioral health, and outpatient visits, which they’ve seen used appropriately in the past two years.
Kasper outlined some learnings from NC Medicaid around telehealth usage during the pandemic as well. What stood out for her team is that clearly, telehealth is a critical tool, and not every visit requires an in-person component. Flexibility in usage and payment will enhance everyone’s experience. However, with two years of data from the pandemic, they found that most users of telehealth lived in urban areas and were white. Kasper noted that telehealth can certainly help overcome issues around social determinants of health, but that the state needs to spend more time thinking about how to be more intentional in promoting telehealth usage through policy to drive health equity.
"Telehealth is not virtual care. It is real care delivered virtually. Why does it matter how the care is delivered when we have an opportunity to step outside of boundaries?"
Representative Adcock took a holistic stance on telehealth, noting “We have to think about the big picture and having infrastructure. Social determinants of health are important to consider.” She acknowledged that coalitions are important in supporting covered services, but that only takes us so far. Really vulnerable people depend on telehealth, and many people are homebound or cannot afford to drive several hours to a doctor's visit. She also encouraged the audience to move away from framing telehealth as virtual care: “Telehealth is not virtual care. It is real care delivered virtually. Why does it matter how the care is delivered when we have an opportunity to step outside of boundaries?”
Reducing administrative burden
When thinking about provider and administrative burden, one of the first areas of reform anyone working in a clinical setting will bring up is the workload associated with prior authorizations. When accountable care organizations like those participating in Aledade’s model are in a total cost of care arrangement centered around value-based care, those independent practices are financially responsible for ensuring positive outcomes in the patient.
Dr. Cohen noted that micromanaging these doctors, practices, and ACOs through prior authorizations and other restrictions is counterproductive to the work that the physicians do, especially in this value-based model. Financial accountability on quality and cost in the ACO model allows payers to rethink other administrative actions they have previously implemented to try to control costs.
What role can the State play?
Kasper at North Carolina Medicaid shared her thoughts on the work Medicaid is doing to support independent primary care practices through value-based models. She acknowledged that this work is happening in a challenging environment, including workforce shortages and a pandemic, and that value-based payments are needed to provide support in this shared goal without additional burden.
Medicaid is also looking into strategies to encourage value-based payment and make value-based arrangements work for providers, including reducing administrative burden and payment flexibilities. In general, the goal is to increase the number of providers caring for the Medicaid population. These plans are intended to support that goal and encourage this outcome, but it is critical to have the appropriate payments and flexibilities. Workforce shortages are cited as NC Medicaid’s top issue, and they are looking to address this in a number of ways – offering better rates, more flexibility in staffing, and mitigating administrative challenges. They are also exploring a number of other solutions and levers, such as funding different workforces like community health workers, doulas, etc.
What role does the legislature play?
Representative Adcock highlighted that the legislature is there to address problems that arise, when the legislators understand the problems. She noted there are many well-intentioned legislators and staffers who have many priorities but may not be experts in the nuances of value-based care and the challenges of independent primary care. She noted that most professional groups ask her what she can do, but that the real question is how we as advocates can help the legislators understand the problem in a solvable manner.
What role can physicians as advocates play?
Representative Adcock’s advice: “You don’t make a big ask until you have a relationship. Get to know us, bring us to your practice, show us what you’re talking about.” We are close to the election; starting January 2023, there will be an entirely new group of legislators to work with. It is important that we demonstrate the value of Aledade’s work, and why they should support it.
No one can expect folks who do not live and work day in, day out in primary care and value-based care to understand the value of the work. Aledade is committed to working with practices and health centers to help facilitate these relationships, and highlight the important work that our independent and community-based clinicians are doing.
How can I get involved?
Click here to learn more about Aledade’s state policy work, and if you are interested in learning more about policy work in your state, reach out to Rebecca Cooper (rcooper@aledade.com).



