Pershing Health System (PHS) is a critical access hospital located in Brookfield, Mo. “We are the only hospital within a 30-mile radius,” Kelly Schwager DNP, NP-C, Director of Rural Health Clinics at Pershing Health System, said.
As the primary caregivers for populations in Healthcare Provider Shortage Areas (HSPAs), the same is true for most Rural Health Clinics (RHCs). Due to funding limitations, workforce shortages and patient transportation barriers, RHCs face their fair share of challenges.
Founded as a not-for-profit hospital more than 50 years ago, PHS provides a full spectrum of primary and secondary health care services to its local and surrounding communities, including an emergency department (ED), inpatient care, skilled nursing services, outpatient surgery, rehabilitation services, and imaging.
To optimize their workflows and get rewarded for the high-quality care they excel at delivering, the team at Pershing Health System joined Aledade for the 2022 Medicare Shared Savings Program (MSSP) performance year.
“We started working with Aledade approximately four months before our official ‘go-live’ date,” Schwager said. “We began educating ourselves on annual wellness visits (AWVs) and their components before implementing new processes as well as new staff.”
Throughout the implementation period, Schwager met regularly with Aledade’s Practice Transformation Specialists who explained what Aledade is, how the partnership would work and the benefits that Pershing Health System could incur.
Success starts with staff collaboration.
“In order to make sure our new commitment with Aledade was a successful one, I knew we would need to add staff to take on the new processes being added to our day-to-day operations. Like many healthcare institutions, finances were tight, and we would have to be strategic in how these processes would happen,” Schwager said.
“One of my Patient Service Representatives voiced interest in learning these new roles. With the immediate success in implanting the new annual wellness visit (AWV) process, her position grew into full-time quickly. She currently does all of our AWV pre-visiting planning, which also includes keeping providers informed on what care gaps need closed as well as diagnosis resolution.”
By resolving much of the necessary prep work before the visit, the clinicians were able to spend less time searching for data in the electronic health record (EHR) and more time reviewing important preventive care measures and discussing care plans with their patients.
After streamlining AWVs for six months, Pershing Health System then added Transition of Care (TOC) workflows, and six months later, Chronic Care Management (CCM). Currently, their nurse manages 50-60 CCM patients monthly.
Maintain a focus on quality patient care.
As an RHC, their focus is still the delivery of primary care services, yet operating as a walk-in clinic, too. In a walk-in clinic model, these opportunities did not exist, explained Schwager.
“Continuity of care was difficult because we were not able to schedule follow-up appointments. We informed the patients when to return and had to trust they would be compliant. Shortly after I became the RHC Director, I implemented our current scheduling model to more of a traditional family practice scheduling procedure.”
PHS is now able to schedule follow-up appointments months in advance, as well as keep open appointments hourly for each clinician to accommodate acute illness walk-in patients.
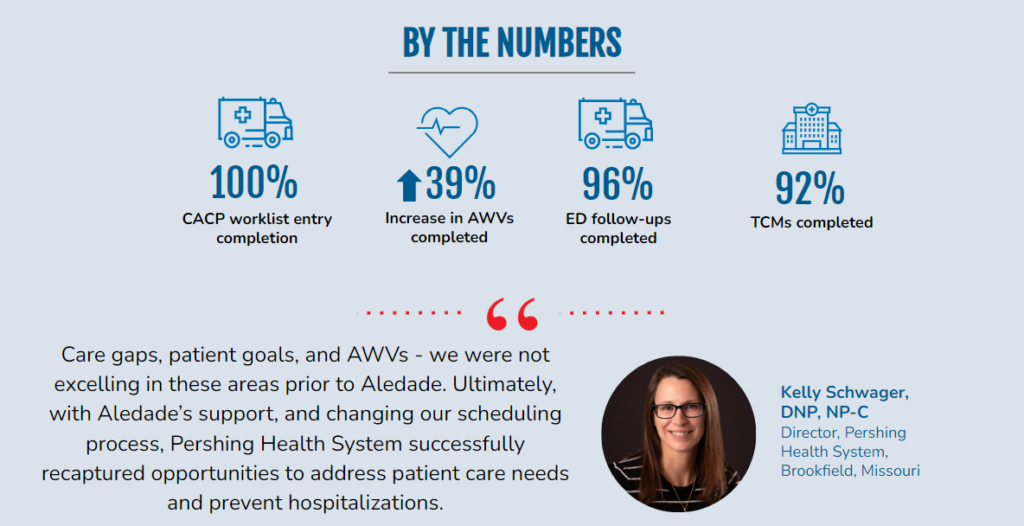
“Care gaps, patient goals, and AWVs – we were not excelling in these areas prior to Aledade. Ultimately, with Aledade’s support, and changing our scheduling process, Pershing Health System successfully recaptured opportunities to address patient care needs and prevent hospitalizations,” Schwager said.
The dedication and teamwork at PHS has been beneficial to their patients: In the 2022 performance year, Pershing Health System achieved 96% emergency department (ED) follow-up; 92% transitional care management (TCM) outreach, ensuring high-risk patients receive the care they need; and 100% comprehensive advanced care planning (CACP) worklist entry completion, allowing patients to align their values and preferences with future care. They also increased their AWV completion rate by 39%.
“With our growing clinics, we are hoping to earmark some of the shared savings to expand our walls in the future,” Schwager stated.
Plan ahead to start your journey in value-based care.
Schwager has recommendations for other RHCs considering joining an ACO:
- Plan carefully. Success in the value-based care model requires strategic thinking and a realignment of job responsibilities to incorporate streamlined and efficient workflows.
- Make sure staff is prepared. Resolve anticipated problem areas before unveiling change to staff.
- Know that ACO participation is a commitment. Be prepared to put in effort to earn shared savings.
- Success will not happen overnight, or perhaps not even in the first year. Getting staff, systems, and workflows aligned takes time.
- Pass the knowledge forward. Trust the Aledade support team to help staff adopt and implement the required changes.
Two years after taking on the role of director, Schwager has witnessed Pershing Health System’s continued success. Now, instead of owing Medicare money at the end of the year, the RHC is earning shared savings and planning for future projects, expansions, and more staff to better support the local community.
Is your rural health clinic ready to take the next step? Reach out to your local ACO leadership to learn how Aledade can support your mission to deliver quality, coordinated care to your rural community.



