By Casey Korba, Director of Policy
The 2022 Physician Fee Schedule, while not earth shattering considering it was written during a time of transition at the start of a new administration, has some key takeaways. In this blog, we outline what you need to know, as well as emphasize where we’ll be focusing our attention and advocacy efforts for the improvements and refinements we need in 2023.
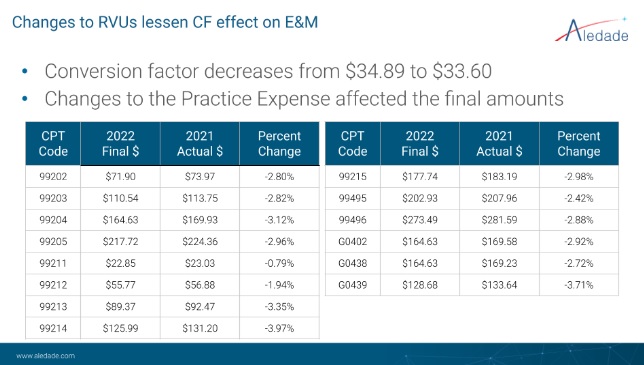
Updates to Payment Rates
The pandemic led Congress to provide some stimulus funding (3.75% increase) for 2021. That will expire soon, though there is still the possibility that Congress could act to extend the funding before the end of the year. The increased valuations of Evaluation & Management (E&M) services remain, and these payments will be 7% higher in 2022 than in 2020. Overall, primary care services (E&M, Annual Wellness Visits, Transitional Care Management) will be 6% higher on average in 2022 than in 2020 but about 2.8% lower than in 2021. MIPS bonuses for non-risk-taking ACOs (1-1.87%) or Advanced APM bonuses (the 5% lump sum) for risk-taking ACOs are in addition to these payments. (MIPS and AAPM for 2022 are based on performance year 2020).
The takeaway: Even with the decrease, there is still an increase in E&M service payments because of the reweighting of the codes finalized in 2020 and implemented in 2021.
Shifting over to the rates: The final PFS rates are a slight decrease from what CMS had proposed. In the final PFS, the changes to the Practice Expense Relative Value Units (RVUs) affected the final amounts.
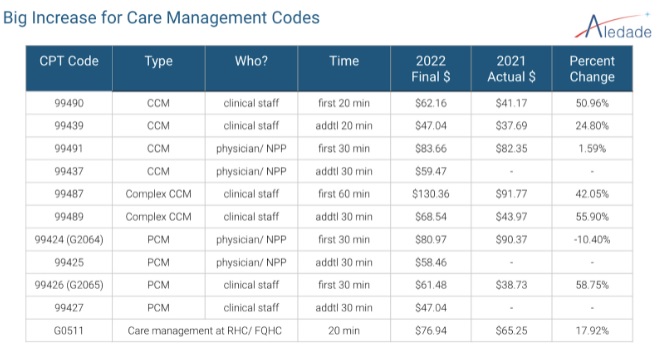
CMS Recognizes Chronic Care Management (CCM) as a Critical Tool for Primary Care
Aledade has long applauded CMS for continuing to evolve CCM over the last six years. For 2022, CMS finalized that all G codes move to AMA CPT codes. Principal care management (single, intense disease) has joined CCM. And, both staff time and physician/NP/PA/CNS time are recognized. Most notably, care management code payments will see a 32% increase, on average, in 2022.
The takeaway: Aledade will be updating its CCM materials with the updated codes.
Medicare Shared Savings Program
Most of the action in MSSP in the PFS is around quality reporting. CMS had proposed moving to all-payer, all-patient reporting for three measures: Diabetes HbA1c Poor Control (ID #001), Screening for Depression and Follow-Up Plan (ID #134) and Controlling High Blood Pressure (ID #236). It is clear from the responses to the proposed rule that CMS had underestimated both the difficulty and accuracy of all-payer, all-patient reporting, and in the final rule, the agency delayed the requirement until PY 2025. ACOs have the option to report the 10 measures in the CMS Web Interface using a sampling of Medicare beneficiaries.
The takeaway: Aledade uses this sampling option as it is far more reflective of the quality of care provided. The delay in the final rule gives us time to have an informed decision-making process on how to best get accurate all-payer, all-patient reporting: What is the best way to measure quality in an ACO? Should we go all-payer? How do we address equity issues? The end goal should be holding everyone to the same standards and not creating a financial incentive to improve quality scores by avoiding patients who need care the most. Is sampling simply more accurate than the total population will ever be? Should we move to 100% claims measures? Have we left too many process measures behind? This will be a hot topic over the next two years.
Rural Glitch and Risk Cap: Missed Opportunities for CMS
Request for information (RFI) is a common tool used by the government to collect information. In the case of ushering in much-needed solutions for the rural glitch and risk cap, this RFI period is a missed opportunity. While many, if not most, ACOs would carry on with the status quo, there are too many ACO outliers who will be harmed by not acting to improve on the misaligned financial incentives. Those of you who are not new to Aledade have heard us describe the urgency of fixing the rural glitch before: for ACOs with large market share (often in rural areas), if they succeed in lowering costs, they lower costs for the entire region. Their regional trend comes down, which essentially means they are penalized for lowering costs.
For the risk cap, if an ACO’s risk score goes up 6% and the region’s risk score goes up 6%, the ACO’s benchmark is reduced by a devastating 3% even though they simply matched their region. Again, for many ACOs this is okay, but for some outliers this will be a big disincentive. The shared goal is to create strong incentives to continue to allow ACOs and the MSSP to thrive, and the current policy runs counter to that goal.
The takeaway: The overwhelming majority of ACOs and stakeholders, including Aledade, made clear in the comment period that it’s long past time to fix these issues. Now, we look to 2023. Expect to hear more from us and others about this issue.
Telehealth: Stable for Now, but Watch this Space for More Changes
The Public Health Emergency (PHE) remains, and CMS continues to take advantage of the flexibilities for telehealth that Congress granted during the pandemic. The category 3 codes that CMS allowed for telehealth will continue through 2023. Additionally, CMS adopted coding and payment for a longer virtual check-in service on a permanent basis.
CMS has made permanent the mental health services provided via telehealth, including getting rid of the geographic restrictions. Patients must come in for an in-person visit once every 12 months (up from 6 months in the proposed rule), and the in-person services and telehealth services must be provided by clinicians in the same specialty and in the same practice. CMS also finalized its change to the definition of interactive communications, which means that audio-only is allowed for mental health telehealth visits. The clinician must document that the patient is not able to get on video or that the patient prefers audio-only.
The takeaway: The pandemic pushed telehealth progress along, but Congress will still need to act to keep some of the other flexibilities allowed during the PHE. We expect more attention on telehealth in 2022.
Closing Thoughts: Physician Fee Schedule Season Continues
The final rule is out and the summaries and takeaways are plenty. We know what work we have ahead of us in the coming months to prepare for the 2023 PFS season. For the next month, Congress is focused on negotiating and passing the reconciliation bill, dealing with the debt limit and continuing to fund the government. However, Aledade and our partner stakeholders are ready to turn the attention and urgency back to value-based care in 2022. We will also continue engaging with CMS and CMMI to keep our key priorities top of mind.



