By Casey Korba, Director of Policy
Longitudinal primary care team support is critical for dual-eligible beneficiaries and can generate savings.
Dual-eligible beneficiaries are individuals who are enrolled in both Medicare and Medicaid by virtue of age or disability, along with meeting income criteria. There are about 12.5 million dual-eligible beneficiaries, and these individuals tend to have complex care needs and health-related social needs that affect daily living.
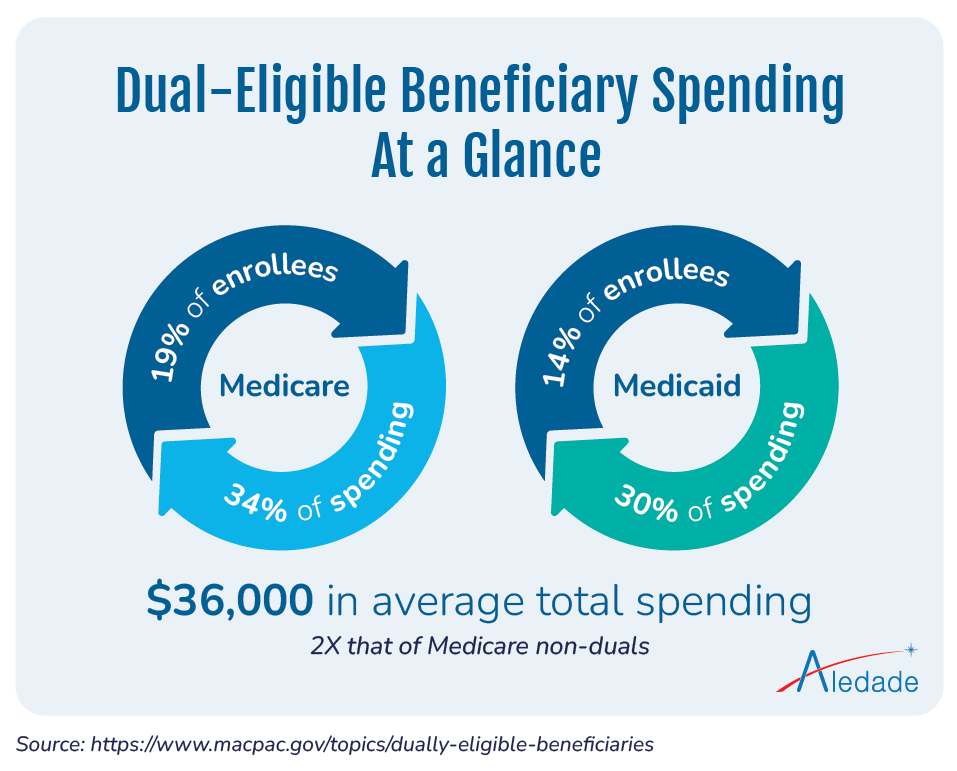
Dual-eligible beneficiaries account for a disproportionately high rate of spending for both Medicare and Medicaid programs. In Medicare, they make up about 19% of enrollees and account for 34% of spending; while in Medicaid, they account for 14% of enrollees and 30% of spending. The average total spending for dual-eligible individuals is more than $36,000 per beneficiary. This is more than double that of Medicare non-duals.
At Aledade, our mission centers around the belief that the best model for patients is a long-term relationship with their primary care team. This is important for everyone but is especially critical for vulnerable patients with complex health and social risk factors.
Unfortunately, the dual-eligible population has been traditionally underserved. This is in part due to primary care workforce shortages, coupled with the challenges of meeting the more complex and intersected health-related social needs of this population. There is a great opportunity to provide dual-eligible beneficiaries with high-quality primary care and substantively improve their health and quality of life.
Aledade’s patient-centered approach helps to improve health outcomes and generate savings.
Aledade has a proven track record of helping independent practices and community health centers (CHCs) provide dual-eligible patients high-value services that can reduce costly emergency room visits and hospitalizations.
In the 2022 performance year, Aledade accountable care organizations (ACOs) achieved a shared savings rate of 13.8% for dual-eligible beneficiaries in the Medicare Shared Savings Program, which is almost double our rate of savings of aged non-dual-eligibles. In Louisiana, one Aledade ACO received a shared savings rate of 26% from their dual-eligible population. Aledade member CHCs in California are responsible for the care of approximately 8,000 dual-eligible patients and achieved a shared savings rate of 12.9%.
Aledade has programmatic and policy solutions to help address challenges in payment structures and care coordination.
We recognize there are many barriers to engaging and improving the health of dual-eligible beneficiaries. The payment structure for dual eligibles is both through federal Medicare and state Medicaid programs. The coordination of these two payment structures is complicated, to say the least. This complexity often leads to fragmented, uncoordinated care, resulting in poor outcomes along with higher costs and inefficient spending for CMS and states.
Every stakeholder remotely connected to the health care system knows how social drivers of health can impact patients’ ability to access care. Retaining these dual-eligible beneficiaries in the practice can be especially hard when they transition out of Medicaid. Losing coverage is usually temporary and based on administrative issues (e.g., complex renewal processes, short-term income fluctuations). However, Medicaid provides assistance, including cost-sharing, for many services that do not get the same coverage in Medicare. Any amount of copay, even temporary, can be a barrier for this population, and practices have to go through administrative hoops to have these fees waived.
These barriers can understandably seem daunting to primary care practices already stretched thin – but at Aledade, we have best practices and strategies that help practices engage dual-eligible beneficiaries in their care and overcome some of these challenges.
The Core 4

Through Aledade’s Core 4 approach, we deliver actionable data insights to primary care organizations so they can engage patients more proactively through Annual Wellness Visits (AWVs), preventive screenings, high-value referrals and wraparound programs. This approach, paired with support from our field teams and population health tool, equips our ACO members to engage high-risk and harder-to-reach populations.
Patient engagement strategies
Aledade works with almost 200 CHCs, and many are employing engagement strategies that are showing signs of success with their dual-eligible beneficiaries.
- Incentives: Providing incentives for dual-eligible beneficiaries to complete their AWVs is one strategy. Practices are able to offer small incentives such as gift, gas, or grocery cards, as an incentive to receive this important service.
- Transportation support: Because transportation is often a barrier, some of our member practices and CHCs are helping patients schedule rideshares and covering the cost. One member practice in Arkansas has set up their own transportation program, working within the applicable regulatory parameters to ensure patients can receive medically necessary care.
In Delaware and Maryland, through Aledade’s pilot program, ACO members can offer Lyft rides to Medicare patients who need help getting to medical appointments – and are able to schedule and pay for rides for beneficiaries. Aledade is exploring offering the program in other markets and business lines in the coming months.
- Community-based partnerships: Many of our independent practices and CHCs are collaborating with community-based organizations (CBOs) to address social drivers of health, including transportation, food insecurity, and connecting patients to community resources. We highlighted some of these best practices in our recent report, and CMS has put out a request for information in the 2024 Proposed Physician Fee Schedule to identify strategies ACOs are using to establish relationships and partner with CBOs.
Providing excellent care for dual-eligible beneficiaries aligns with Aledade’s mission to do what is good for patients, good for practices, and good for society. Dual-eligible beneficiaries are some of the most vulnerable patients managed by Aledade member practices. The complex needs of this population require the kind of coordinated, holistic, “quarterbacking” care that only value-based primary care practices can provide.
By prioritizing the care of these beneficiaries, we can help improve health outcomes, reduce disparities, enhance shared savings, and ensure the success of our ACOs.



